Abstract
Introduction
While prior studies suggest that mental health complications are underdiagnosed and undertreated in patients with cancer, a paucity of data exists for patients with diffuse large B-cell lymphoma (DLBCL). Indeed, mental illness can impact the success of potentially curative treatment for DLBCL including delays in treatment initiation, poor chemotherapy compliance, and suboptimal rates of completion. Accordingly, we aimed to examine the risk of incident mental health events following DLBCL diagnosis, and the association of mental health conditions with overall survival (OS).
Methods
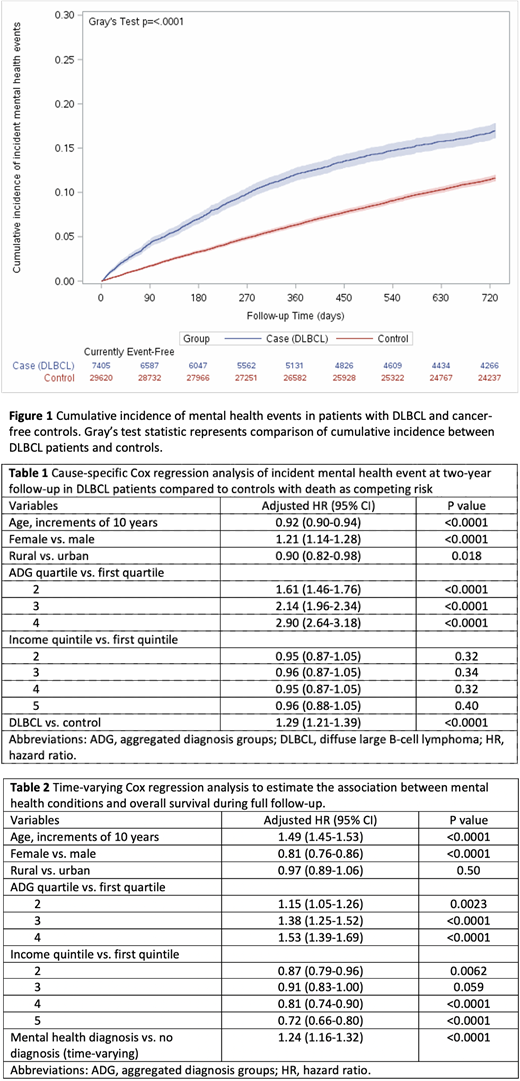
We conducted a population-based observational study using linked administrative healthcare databases from Ontario, Canada. All Ontario residents aged ≥18 years with DLBCL treated with rituximab-based chemotherapy for curative intent between January 2005 and December 2017 were identified and followed from the date of first rituximab until March 1, 2020. The primary outcome was any incident mental health event (emergency department visit, hospitalization, or outpatient visit for mood disturbance including depression and anxiety, psychotic disorder, or substance-related disorder). Patients with a DLBCL diagnosis without pre-existing mental health comorbidity in the 2-years prior to start of rituximab were matched to mental health condition- and cancer-free controls in a 1:4 ratio based on birth year and sex. The cumulative incidence function was used to estimate incidence of mental health events while accounting for the competing risk of death, and differences were compared using Gray's K-sample test. A cause-specific Cox regression model was used to estimate mental health events up to two-years following rituximab initiation, while controlling for relevant covariates (sex, age modeled in 10-year interval increments, rural vs. urban residence, income quintile, and quartile of sum of aggregated diagnosis groups (ADGs) as a measure of comorbid disease burden (mental health and cancer diagnoses excluded). The secondary outcome was the association of mental health conditions on OS for all identified DLBCL patients, evaluated using Cox regression (with mental health event as time-varying variable).
Results
We identified 10,299 patients diagnosed with DLBCL and treated with a rituximab-containing regimen in Ontario, with median age 67 years (IQR 56-76), 45.9% female, median ADG score of 9 (IQR 6-11), and median of 6 cycles of rituximab received (IQR 4-6). For patients with available stage data (49.2% of cohort), 34.6% had stage IV at diagnosis. When compared to birth year- and sex-matched controls (n=29,620), DLBCL cases (n=7,405) had a greater comorbidity burden (p<0.001). During a median follow-up of 5.16 years (SD+4.13), 28.8% of DLBCL patients without pre-existing mental health conditions developed an incident mental health event. With adjustment of potential confounders, patients with DLBCL still had significantly higher risk of an incident mental health event compared to controls (adjusted hazard ratio [aHR] 1.29, 95% confidence interval [CI] 1.21-1.39, p<0.0001) (Figure 1, Table 1). Younger age, female sex and higher comorbidity burden were associated with an increased risk of an incident mental health event (Table 1). In addition, having a mental health condition (either pre-existing or after start of rituximab) was associated with a significantly worse one-year OS (aHR 1.11, 95% CI 1.01-1.22, p<0.0001) and at end of follow-up (aHR 1.24, 95% CI 1.16-1.32, p<0.0001; Table 2). Additional factors independently associated with worse overall OS included older age, increased comorbidity, and male sex (Table 2).
Conclusions
In this large population-based study, patients with DLBCL were found to have a significantly higher risk of incident mental health events compared to controls. Moreover, the presence of a mental health condition was associated with worse survival outcomes. These data suggest that patients with DLBCL, particularly those with pre-existing mental health condition(s), would benefit from routine mental health assessment and management during follow-up, not only for mental health itself but also potentially to improve survival.
Prica: Astra-Zeneca: Honoraria; Kite Gilead: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal